4 Human Health and Disease
Human Health and Disease
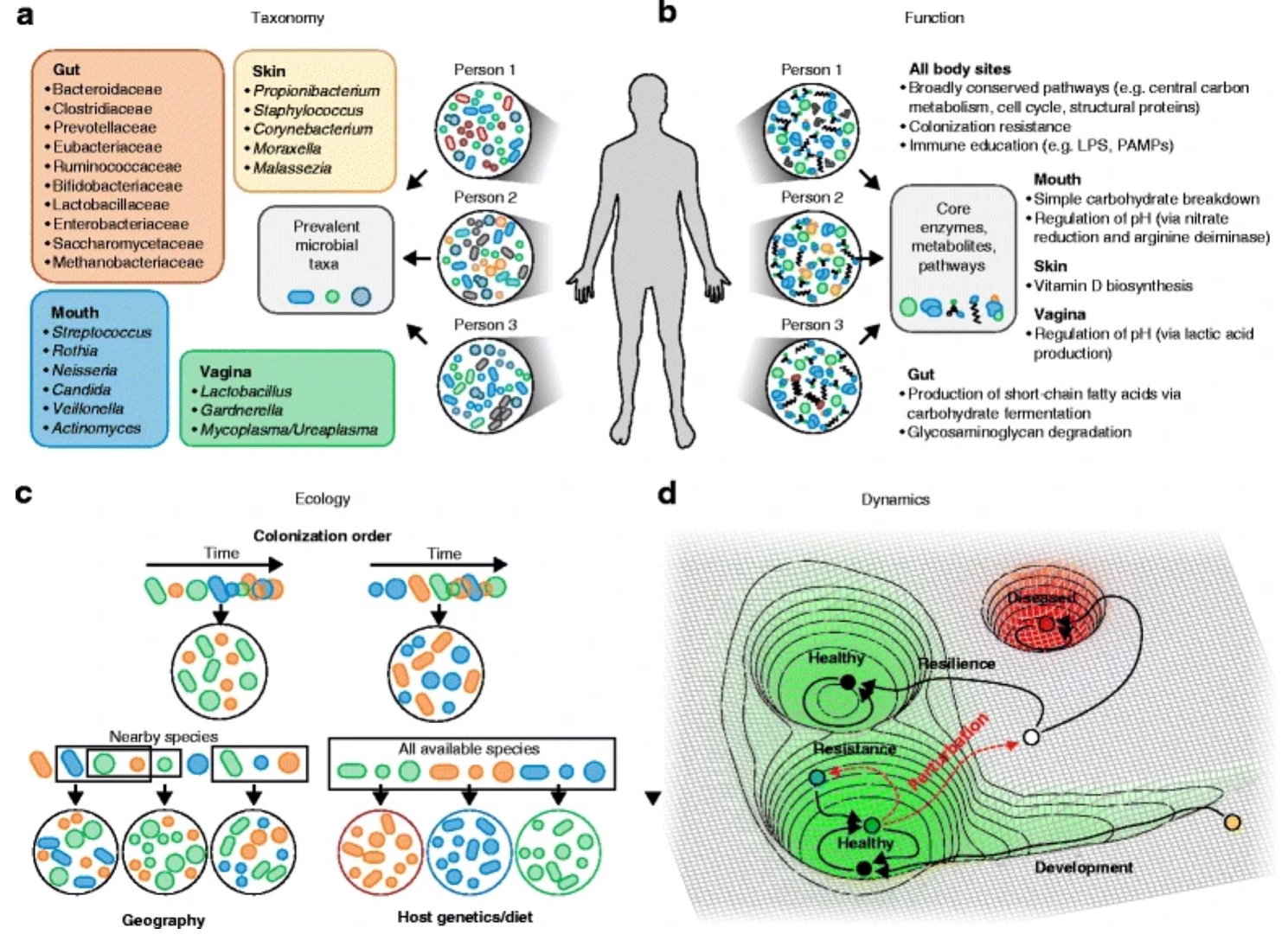
The human microbiome plays a vital role in maintaining homeostasis of various organ systems and protecting against infectious agents. It can be subcategorized into local or regional microbiomes throughout the body, such as the gut, oral, skin, lung, and vaginal microbiomes. These manicured microecosystems are highly organized and complex, with each person having their own distinct makeup and distribution of various microorganisms. Though, individual microbiomes are unique, there is still capacity to understand key role players in the community and their potential for adaptation to improve human health in general.
Disruption, or dysbiosis, of the microbiome can cause serious diseases and allow for opportunistic infections to occur. This disturbance can be caused by a variety of factors including changes in diet, exercise, geographical location, age, habits, as well as medical intervention like antimicrobial chemotherapy. This change in microbial composition subsequently leads to the development and exacerbation of a number of diseases impacting essentially every aspect of human physiology including the digestive, respiratory, integumentary, central nervous, and reproductive systems. Alternatively, dysbiosis may be the result of a particular disease, and in other cases disease-dysbiosis may be bidirectional (Silverman et al., 2019). The human microbiome can be influenced by many of the above mentioned factors, but also others like life partners, pet ownership, and occupation, which do not necessarily correlate with or contribute to dysbiosis (Kiecolt-Glaser et al., 2019, Kates et al., 2020).
A major driving feature of many of these elements is the host’s genetics, which can also directly impact their microbiome (Tabrett and Horton, 2020). Part of the gut microbiome and even individual types of bacteria have been shown to be heritable (Kurilshikov et al., 2017), and it is likely that other areas of the human microbiome, like the skin microbiome, could be passed from parent to offspring as well (Si et al., 2015). The host genotype is intimately linked to its microbiome and has been shown to affect dysbiosis-induced diseases such as inflammatory bowel disease and atopic dermatitis (Knights et al., 2013, Dabrowska and Witkiewicz, 2016, Woo and Sibley, 2020). Host genetics and their microbiome can even indirectly affect one’s susceptibility to other diseases. For example, the attractiveness of mosquitos to particular individuals is an heritable trait which is influenced by the many factors, including the skin microbiome; therefore altering the potential of contracting a mosquito-borne pathogen, such as a Plasmodium parasite which causes malaria (Martinez et al., 2020). It seems there is a combination between environmental factors, host genetics, behavior, and others that continually build and adapt the human microbiome, however, is worthy to note that the former may play a larger role in shaping particular microbiomes, such as the gut microbiome (Rothschild et al., 2018).
Media Attributions
- Figure 1 – Possible definitions of a healthy microbiome: composition, function, dynamics, and ecology by Lloyd-Price et al., 2016 adapted by Dylan Parks. Licensed under Creative Commons Attribution 4.0 International License http://creativecommons.org/licenses/by/4.0/
- Video 1 – You have the microbiome you deserve by Research Square. Licensed under Creative Commons: By Attribution 3.0 License https://creativecommons.org/licenses/by/3.0/
References
- Dąbrowska, K., & Witkiewicz, W. (2016). Correlations of Host Genetics and Gut Microbiome Composition. Frontiers in Microbiology, 7, 1357. https://www.frontiersin.org/article/10.3389/fmicb.2016.01357
- Kates, A. E., Jarrett, O., Skarlupka, J. H., Sethi, A., Duster, M., Watson, L., Suen, G., Poulsen, K., & Safdar, N. (2020). Household Pet Ownership and the Microbial Diversity of the Human Gut Microbiota. Frontiers in Cellular and Infection Microbiology, 10, 73. https://www.frontiersin.org/article/10.3389/fcimb.2020.00073
- Kiecolt-Glaser, J. K., Wilson, S. J., & Madison, A. (2019). Marriage and Gut (Microbiome) Feelings: Tracing Novel Dyadic Pathways to Accelerated Aging. Psychosomatic Medicine, 81(8), 704–710. https://doi.org/10.1097/PSY.0000000000000647
- Knights, D., Lassen, K. G., & Xavier, R. J. (2013). Advances in inflammatory bowel disease pathogenesis: linking host genetics and the microbiome. Gut, 62(10), 1505. https://doi.org/10.1136/gutjnl-2012-303954
- Kurilshikov, A., Wijmenga, C., Fu, J., & Zhernakova, A. (2017). Host Genetics and Gut Microbiome: Challenges and Perspectives. Trends in Immunology, 38(9), 633–647. https://doi.org/https://doi.org/10.1016/j.it.2017.06.003
- Martinez J., Showering, A., Oke, C., Jones, R. T., & Logan, J. G. (2020) Differential attraction in mosquito–human interactions and implications for disease control. Phil. Trans. R. Soc. B. Biol. Sci, 376(1818), 20190811. https://doi.org/10.1098/rstb.2019.0811
- Rothschild, D., Weissbrod, O., Barkan, E., Kurilshikov, A., Korem, T., Zeevi, D., Costea, P. I., Godneva, A., Kalka, I. N., Bar, N., Shilo, S., Lador, D., Vila, A. V., Zmora, N., Pevsner-Fischer, M., Israeli, D., Kosower, N., Malka, G., Wolf, B. C., … Segal, E. (2018). Environment dominates over host genetics in shaping human gut microbiota. Nature, 555(7695), 210–215. https://doi.org/10.1038/nature25973
- Si, J., Lee, S., Park, J. M., Sung, J., & Ko, G. (2015). Genetic associations and shared environmental effects on the skin microbiome of Korean twins. BMC Genomics, 16(1), 992. https://doi.org/10.1186/s12864-015-2131-y
- Silverman, G. J., Azzouz, D. F., & Alekseyenko, A. v. (2019). Systemic Lupus Erythematosus and dysbiosis in the microbiome: cause or effect or both? Current Opinion in Immunology, 61, 80–85. https://doi.org/10.1016/j.coi.2019.08.007
- Tabrett, A., & Horton, M. W. (2020). The influence of host genetics on the microbiome. F1000Research, 9, F1000 Faculty Rev-84. https://doi.org/10.12688/f1000research.20835.1
- Woo, T. E., & Sibley, C. D. (2020). The emerging utility of the cutaneous microbiome in the treatment of acne and atopic dermatitis. Journal of the American Academy of Dermatology, 82(1), 222–228. https://doi.org/10.1016/j.jaad.2019.08.078

